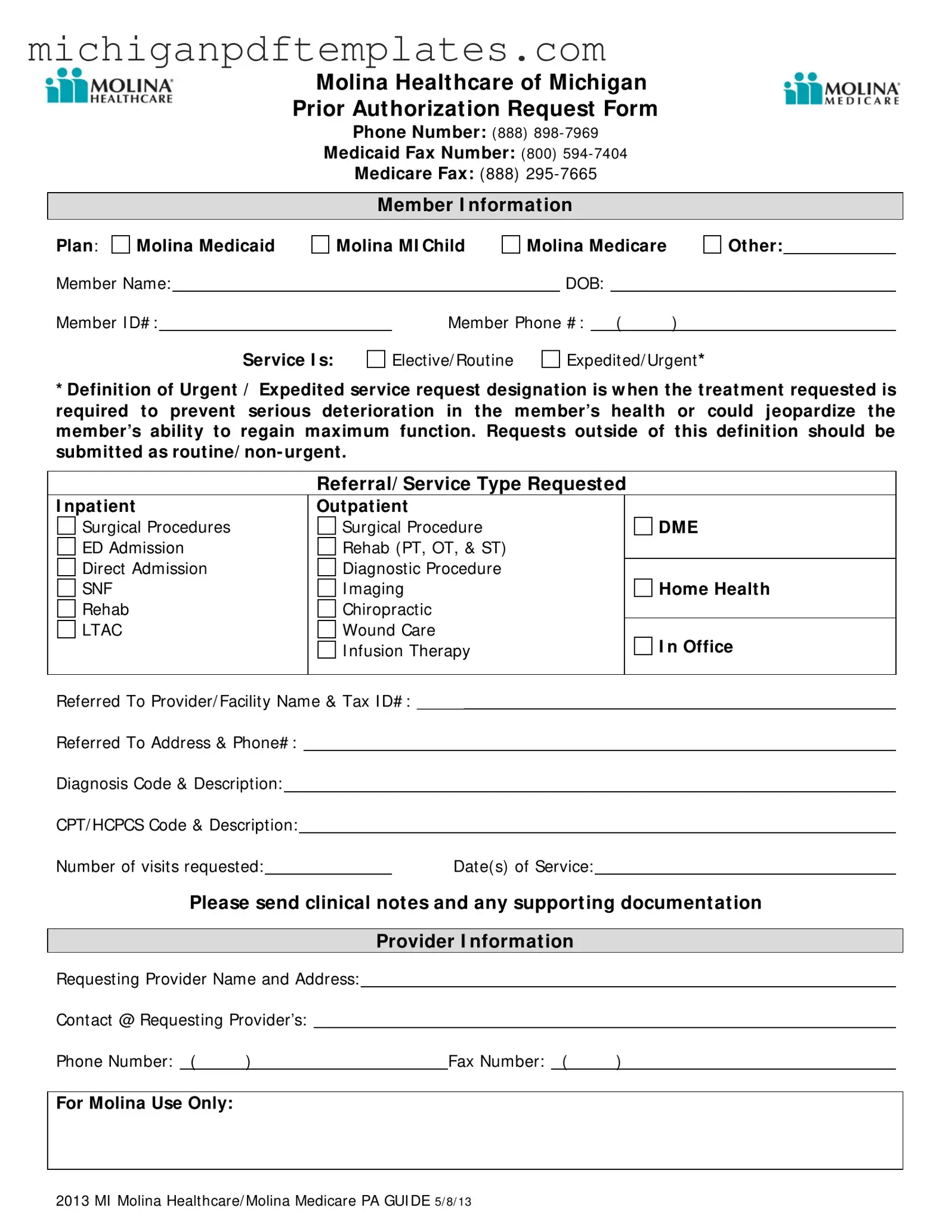
Fill in Your Michigan Molina Prior Authorization Form
The Michigan Molina Prior Authorization form is a crucial document used to request approval for specific medical services under Molina Healthcare of Michigan. This form ensures that necessary treatments are authorized before they are provided, which can prevent delays in care. To initiate the process, fill out the form by clicking the button below.
Get Your Form Now
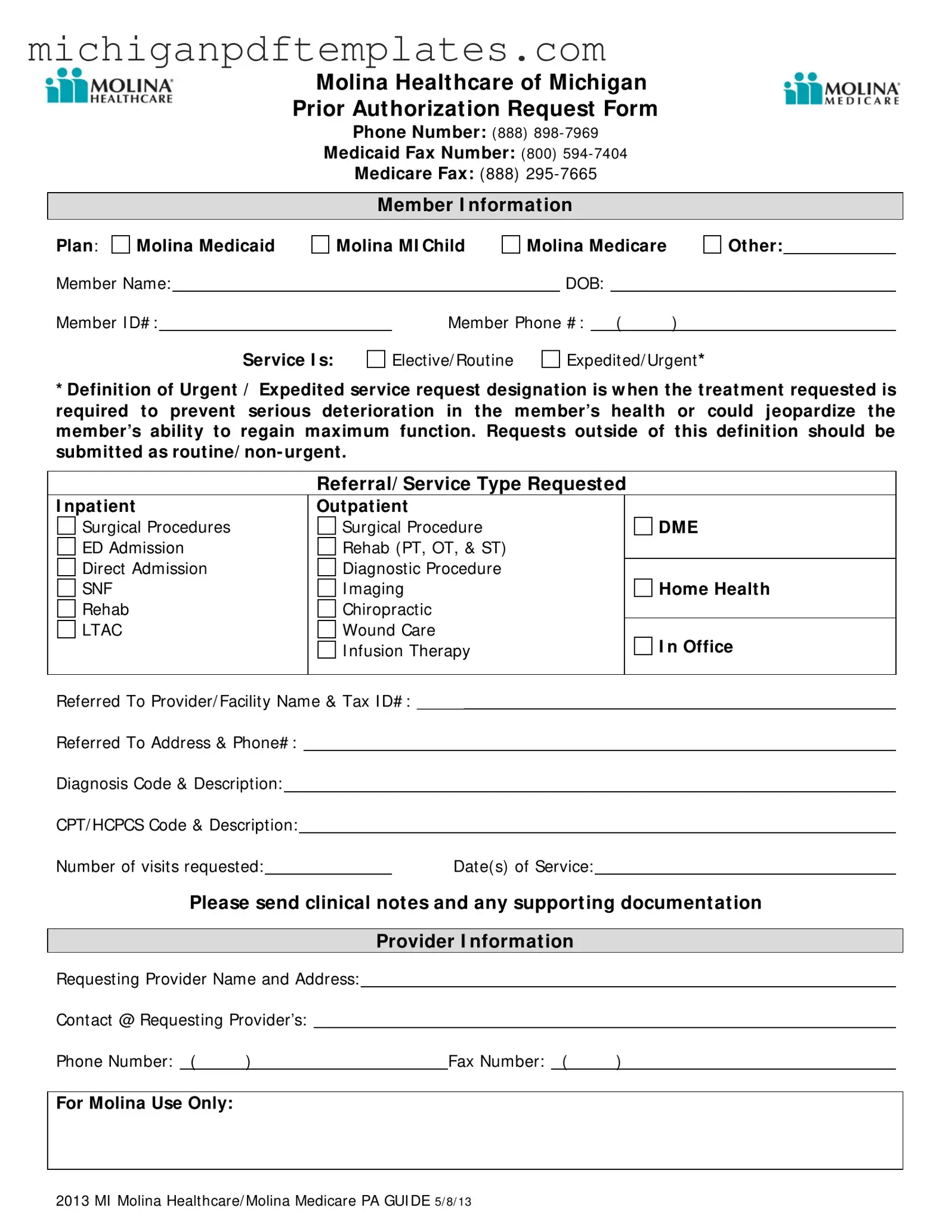
Fill in Your Michigan Molina Prior Authorization Form
Get Your Form Now
Get Your Form Now
or
▼ PDF Form
Finish this form quickly and move on
Fill in and complete Michigan Molina Prior Authorization online quickly.