Fill in Your Meridian Michigan Pre Approval Form
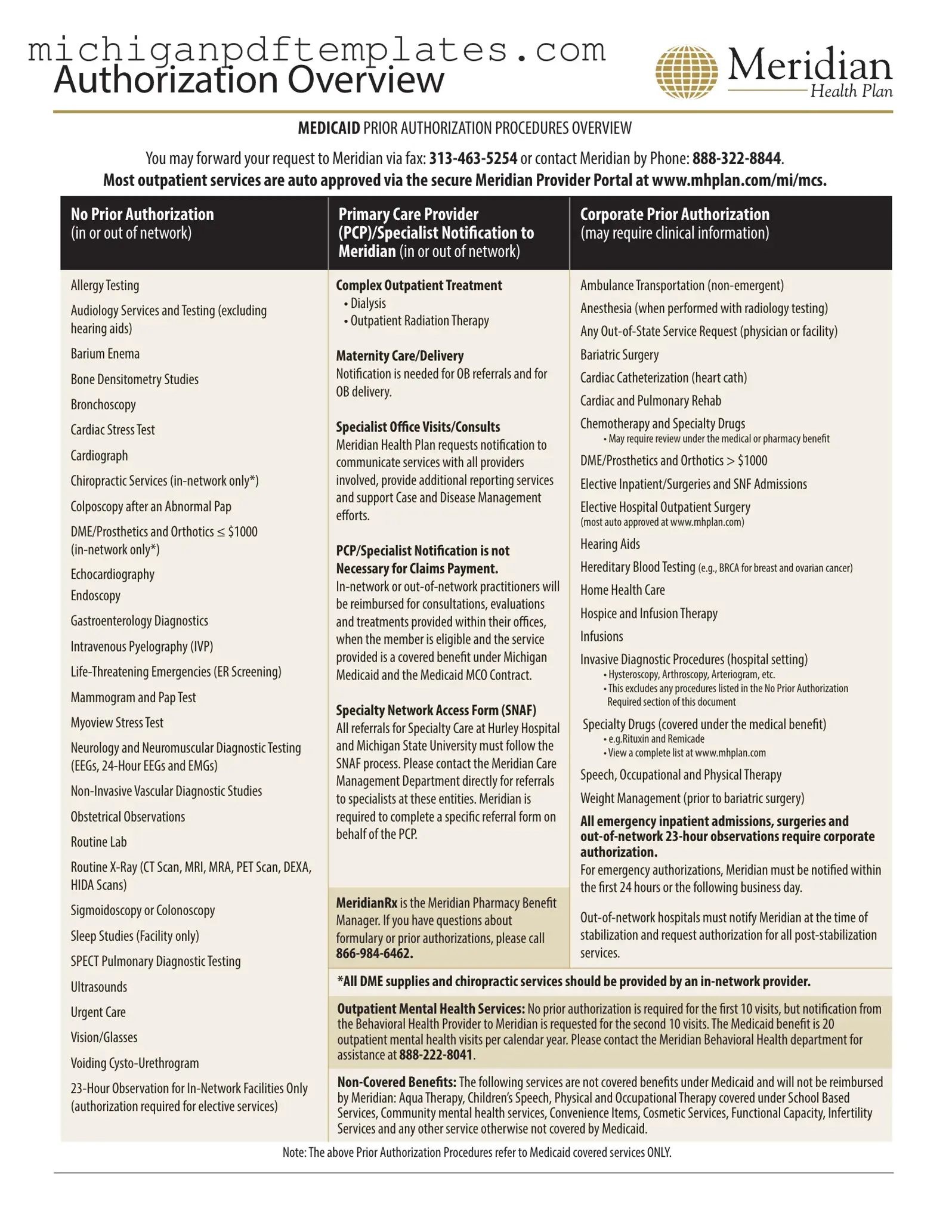
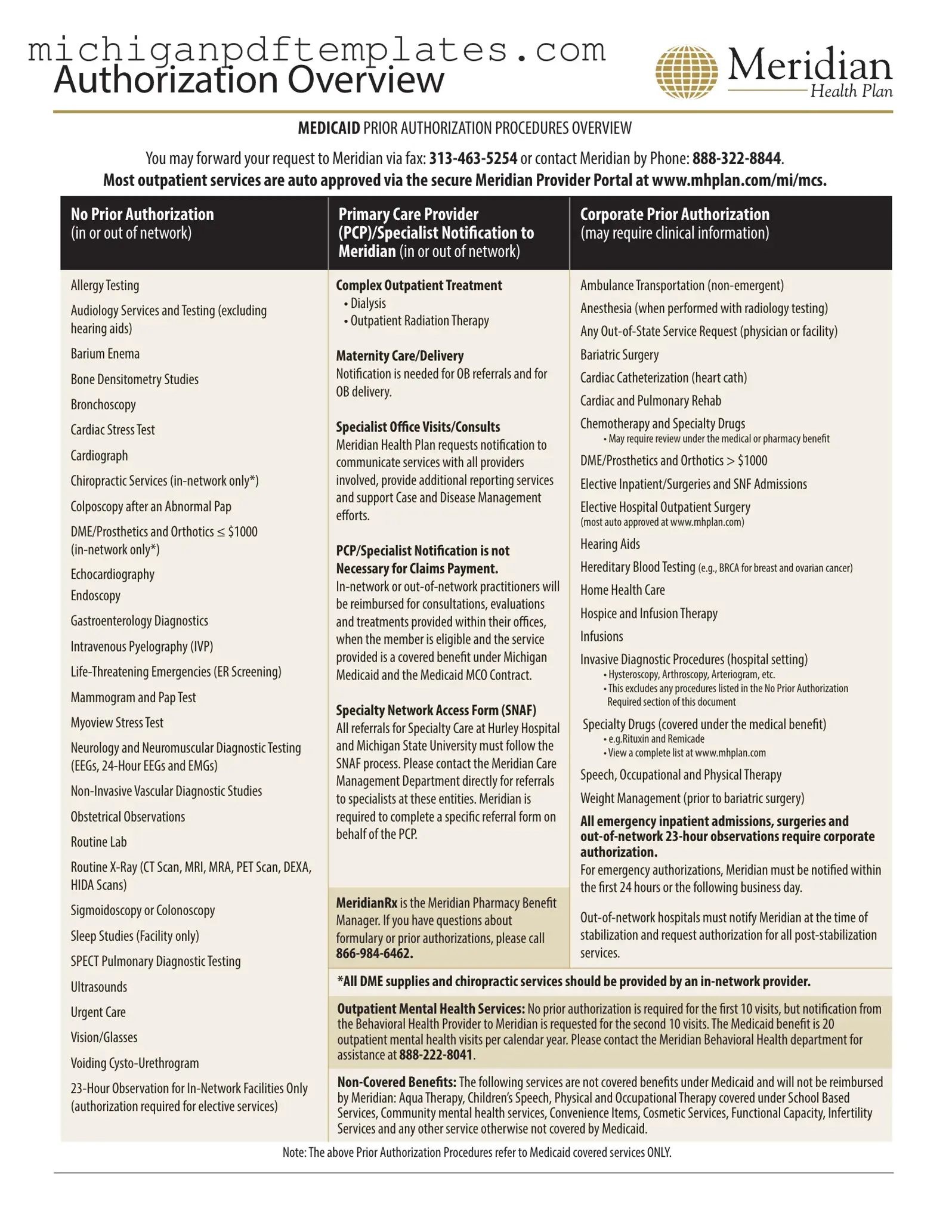
The Meridian Michigan Pre Approval form is a critical document used to obtain prior authorization for various medical services under the Michigan Medicaid program. This form streamlines the process for healthcare providers seeking approval for specific treatments and procedures, ensuring that patients receive timely care while adhering to Medicaid guidelines. To facilitate your request, consider filling out the form by clicking the button below.
Get Your Form Now
Fill in Your Meridian Michigan Pre Approval Form
Get Your Form Now
Get Your Form Now
or
▼ PDF Form
Finish this form quickly and move on
Fill in and complete Meridian Michigan Pre Approval online quickly.