Legal Michigan Do Not Resuscitate Order Template
A Michigan Do Not Resuscitate Order (DNR) form is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. By completing this form, patients can ensure that their preferences for end-of-life care are respected by healthcare providers. If you are considering filling out a DNR form, click the button below to get started.
Get Your Form Now
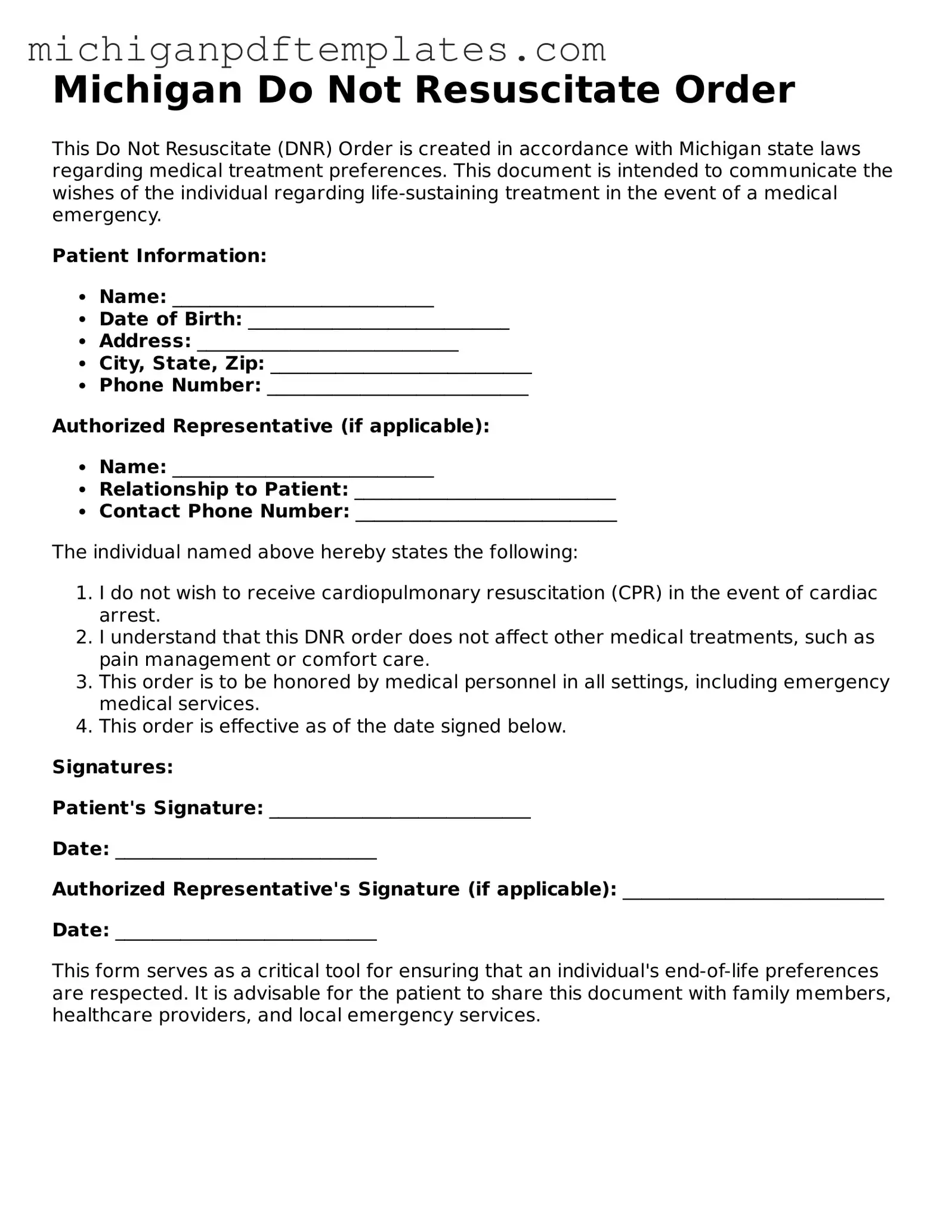
Legal Michigan Do Not Resuscitate Order Template
Get Your Form Now
Get Your Form Now
or
▼ PDF Form
Finish this form quickly and move on
Fill in and complete Do Not Resuscitate Order online quickly.